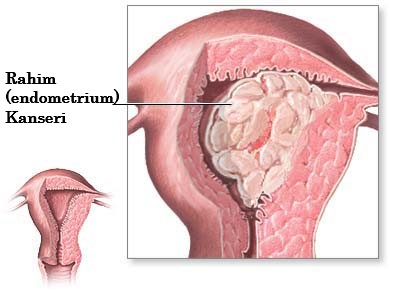
Uterine (Endometrium) Cancer
İçindekiler
- 1 Who Gets Uterine (endometrial) Cancer?
- 2 Factors that reduce the risk of uterine (endometrial) cancer:
- 3 Uterine Cancer Symptoms?
- 4 How is uterine cancer (endometrial cancer) detected?
- 5 Uterine Cancer Treatment
- 6 Staging of Uterine (Endometrial) Cancer (FIGO 2009 staging):
- 7 What will happen after uterine cancer treatment?
Uterine (Endometrial) cancer is the most common gynecological cancer in women after breast, colorectal and lung cancer. Although there is no effective screening test to detect the disease, 75% of them are detected in the initial stages due to early symptoms. Seeing a doctor for vaginal bleeding or spotting after menopause can help detect cancer at an early stage. The 5-year survival rate is around 84% on average for all stages, and this rate is even higher when the disease is caught early.
When uterine cancer (endometrial cancer) is mentioned, cancers originating from the endometrium, which forms the inner layer of the uterus, are understood.
Who Gets Uterine (endometrial) Cancer?
It is especially a disease of elderly and postmenopausal women. 70% of cases are between the ages of 45-74.
Risk factors:
be over 60 years old,
Obesity (obesity)
Long-term use of hormone drugs that do not contain progesterone, but only estrogens,
Menopause starting at a young age and entering menopause at an advanced age,
Never giving birth or a history of infertility
Having a personal or family history of colon cancer or endometrial cancer
History of breast or ovarian cancer
Ovarian diseases
Use of tamoxifen (a hormone drug used in the treatment of breast cancer),
Diabetes (diabetes),
A diet rich in animal fat,
Hypertension (high blood pressure),
They are menstrual irregularities.
Estrogen replacement therapy
Factors that reduce the risk of uterine (endometrial) cancer:
Long-term use of birth control pills reduces the risk, and this protection continues for 10 years after discontinuation of the drug.
Checking with a doctor when heavy, excessive or irregular bleeding develops in menstruating women
Vaginal bleeding after menopause is the earliest sign of endometrial cancer, and should be checked as soon as possible.
Some types of endometrial hyperplasia cases (Complex Hyperplasia with Atypia) tend to turn into cancer if left untreated. In this case, surgical removal of the uterus can prevent this.
If there is Hereditary Nonpolyposis Colon Cancer or if there is an increased risk in this regard, it may be recommended to remove the uterus if the endometrial biopsy has been completed every year since the age of 35, or if the child has been requested.
Since tamoxifen, which is used in the treatment of breast cancer, increases the risk of endometrial cancer, patients should be made aware of this issue and should not disrupt their routine gynecological examinations,
Maintaining a healthy weight, balanced diet, controlling existing diabetes and high blood pressure
There is no screening test to be recommended to detect uterine cancer for women who have no complaints or who do not carry a familial risk for cancer. But most women with endometrial cancer have early symptoms. These symptoms are:
Uterine Cancer Symptoms?
Vaginal bleeding after menopause,
Vaginal bleeding, spotting outside of menstrual periods
abnormal watery, bloody vaginal discharge
Pain or mass in the pelvic area
How is uterine cancer (endometrial cancer) detected?
Abnormal vaginal bleeding, spotting or discharge is especially important in menopausal women. In women who are still menstruating, it is in the form of irregular menstrual bleeding. All women who have bleeding after menopause or who have increased vaginal bleeding after the age of 40 should consult a doctor for the possibility of uterine cancer. In addition, measurement of uterine lining (endometrium) thickness with transvaginal ultrasound during periodic gynecological examinations can also give an idea about uterine cancer. If a thickened endometrium is detected in the postmenopausal years, it should be evaluated for cancer.
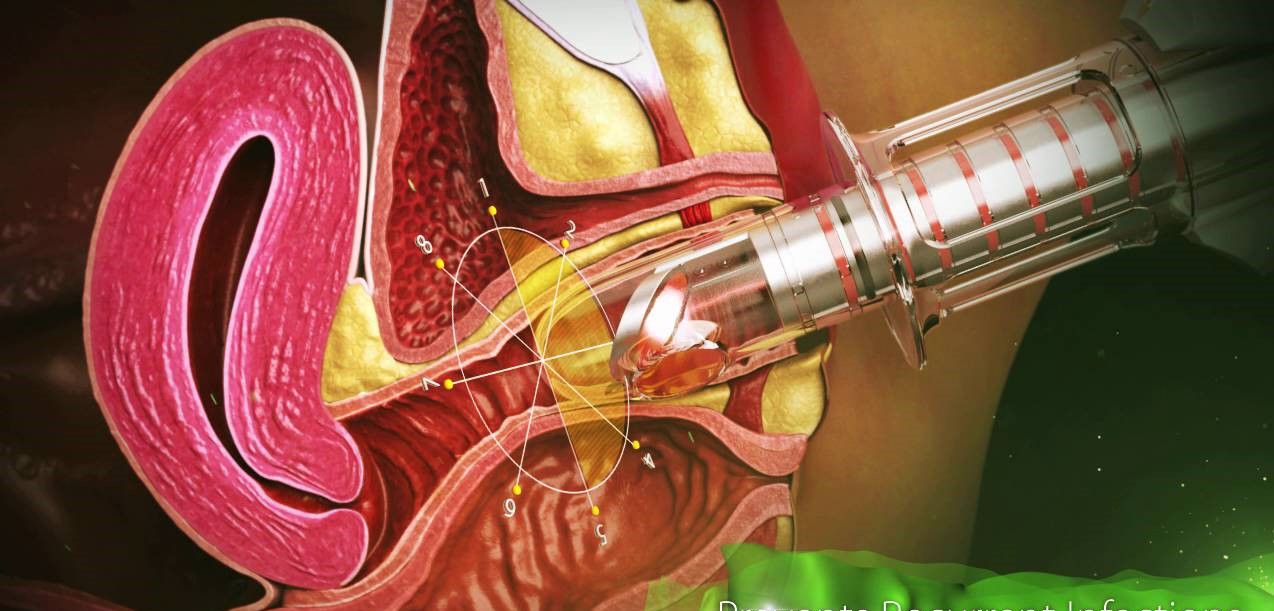
In the presence of any of the above symptoms, a gynecologist should be consulted. When the gynecologist suspects endometrial cancer, he takes some tissue from the uterus through endometrial biopsy or curettage and sends it to pathology. When the piece taken is evaluated by the pathologist, if there is cancer, its type and degree are reported in the report. As the degree of cancer increases, the probability of spread and recurrence of the disease increases.
In the diagnosis of endometrial cancer, imaging methods such as transvaginal ultrasound, computed tomography (CT), magnetic resonance imaging (MRI) and position emission tomography (PET) can also be applied when necessary.
In addition, CA125 increases excessively in endometrium and ovarian cancers, this test can be used to evaluate the patient’s response to follow-up and treatment.
As endometrial cancer spreads, it first progresses to the tubes, ovaries, and lymph nodes. It can also spread to the cervix , vagina, and lungs. Advanced cancer can involve the bladder and large intestine.
75-80% of endometrial cancers are Endometrioid adenocarcinoma. Other types carry an increased risk of recurrence or distant metastasis. The prognosis is poor in adenosquamous carcinoma (6.9%), serous papillary carcinoma (less than 10%), clear cell carcinoma (5.7%), small cell ca (1%). Breast carcinoma is the most common extragenital tumor that metastasizes to the uterus. Stomach tumor, malignant melanoma, lung tumor, colon tumor, pancreatic tumor and kidney tumor may also metastasize to uterus with decreasing frequency.
Uterine Cancer Treatment
When deciding on the treatment of endometrial cancer, the type, grade, stage of the cancer, general health status of the patient and personal preferences are taken into consideration. The aim of surgery in endometrial cancer is to remove as much of the cancerous tissue as possible from the body. Therefore, total removal of the uterus (hysterectomy) is the basic principle. Tubes and ovaries are removed. In very early stage cases (the tumor is limited to the uterus and there is no deep myometrial invasion), only removal of the uterus and ovaries (TAH+BSO) and cytological examination of the peritoneal washing fluid is sufficient. In the remaining stages, a biopsy is performed from the pelvic and paraaortic lymph nodes and the extent of the disease is determined by pathological evaluation. According to the findings, it is planned to add radiotherapy and/or chemotherapy to the treatment in the postoperative period.
Staging of Uterine (Endometrial) Cancer (FIGO 2009 staging):
Stage I Tumor is limited to the uterus
IA: Tumor depth does not exceed half of the myometrium.
IB: There is tumor depth up to or exceeding half of the myometrium.
Stage II: The tumor has spread to the cervical stroma but has not grown outside the uterus.
Stage III Tumor has local or regional spread
IIIA: The tumor has spread to the serosa layer of the uterus and/or the adnexa.
IIIB: There is vaginal and/or parametrial spread.
IIIC: Metastasis to pelvic and/or paraaortic lymph node
IIIC1: Pelvic lymph node spread
IIIC2: Paraaortic lymph node invasion and/or pelvic lymph node involvement
Stage IV: Bladder and/or rectal mucosal involvement, and/or distant organ spread
IVA: Invasion of the bladder and/or rectal mucosa
IVB: Distant metastasis includes intra-abdominal spread and/or inguinal lymph node involvement.
If the cancer has not spread outside the uterus yet, surgical treatment provides a complete recovery.
However, if it has spread to other organs or lymphatic tissues, additional treatment will be required. Radiation (radiation) therapy is applied after surgery in advanced uterine cancers.
Chemotherapy is drugs used to kill cancer cells. The place of chemotherapy in endometrial cancer is limited, these drugs are usually used in combination.
What will happen after uterine cancer treatment?
A check-up is usually recommended every 3 months for the first year after endometrial cancer treatment, and every 6 months for the next 2 years. During the controls, patients undergo a complete physical and pelvic examination, blood tests, pap smear, as well as radiological examinations if necessary. 85-90% of women in the first stage of the disease show no signs of cancer for 5 years after treatment. The chances of a complete recovery are reduced in more advanced stages.
Appointment and Contact Information for Jin.Op.Dr.Yeşim Yerçok (Gynecology and Obstetrics Specialist) :
Phone: +90 216 385 17 15
Address: Fener Kalamış cad. Billur apt. No:5 Da:9 Kiziltoprak – Kadıköy / İSTANBUL
E-Mail:
info@dryesimyercok.com